Poikilocytes are abnormally shaped red blood cells (erythrocytes.) Poikilocytosis is an abnormal number of them in a blood smear. They are commonly seen in anemia and can be very valuable as part of the diagnosis of the exact cause.
The abnormal shapes of poikilocytes are caused either by a membrane abnormality or by cell trauma.
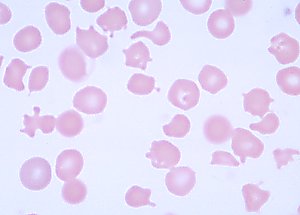
Normal red blood cells are biconcave disc shaped.

Poikilocytes are sometimes seen in babesiosis, during cancer treatment by a drug called doxorubicin, DIC, liver disease in cats, blood turbulence from diseases such as hemangiosarcoma or some types of heart disease, also when anything adversely affects red blood cell production in the bone marrow.
Special care must be taken whilst preparing blood smears as miss-handling or poor technique can damage normal cells & make them look abnormal on the smear. Also overuse of the anti-coagulant EDTA whilst preparing can skew results.
Types of Poikilocytes:
- Acanthocytes: Caused by a cell membrane abnormality. They are also called thorn, spur, spiculated or spike cells & have 5 – 10 spikes. They can indicate thyroid or liver problems and can also be seen after a splenectomy.
- Degmacytes: Caused by cell membrane abnormality. Degmacytes are also called bite cells. One or more semi-circular “bites” have been removed from the cell by the spleen macrophages in an attempt to remove denatured hemoglobin from the cell. Oxidization normally causes this denaturing. For more information including causes see Heinz Body Anemia
- Dacrocytes: Caused by cell trauma. Also called teardrop cells and are often seen in myelofibrosis with myeloid metaplasia, & other retoculo-endothelial disorders, or possibly myelophthisic anemia, or bone marrow infiltration by hematologic or non-hematologic malignancy. Dacrocytes can be caused by the removal of a part of the cell as it travels through the tortuous spleen pathways. To date, it is believed that the red cell membrane may be stretched too far and is unable to go back to it’s usual shape. An error in slide preparation can cause cells to look like this, but their tails would all point in the same direction! True dacrocytes would have tails pointing in various different directions.
- Echinocytes: Caused by a cell membrane abnormality. Echinocytes are also called berry, burr or crenated cells. Echinocytes have 10-30 spiny projections and can indicate malnutrition or kidney failure. Miss-handling of a blood smear preparation, i.e. too much EDTA, can make cells look like echinocytes, when it is actually a laboratory preparation error. Doing another slide is therefore recommended to confirm or deny their presence.
- Elliptocytes & ovalocytes: Caused by a cell membrane abnormality. These elliptical shaped cells can indicate various types of anemia, hereditary elliptocytosis, iron deficiency anemia, infectious anemia, thalassemia & are also seen in the new-born.
- Keratocytes: Caused by cell trauma. They are also called horn cells & are shaped like a spindle or a half moon. They are a very important indicator for DIC. Possible causes:
- DIC
- Glomerulonephritis
- Hemangiosarcoma (often with DIC)
- Hepatic diseases
- Iron deficiency anaemia
- Hemolytic anaemia
- Lymphosarcoma
- Neoplasia (sometimes with DIC)
- Vascular prostheses such as a graft
- Microspherocytes: Caused by cell trauma & are seen in hemolytic jaundice. They are small spherocytes.
- Pyropoikilocytes are types of poikilocytes caused by cell trauma & are seen in hereditary anemia characterised by hemolytic anemia.
- Rouleaux – not strictly a miss-shapen cell (poikilocyte), but relevant as you may see them reported on your pet’s blood smear. Red cells almost “form a line” & look like a stack of coins because the cells are aggregating or sticking together – seen in anemia, infections, inflammatory diseases, diabetes mellitus, multiple myeloma, cancers & macroglobulinaemia (seen in lymphoplasmacytic lymphoma), also seen when plasma protein concentration is increased & when erythroid sedimentation rate is high.
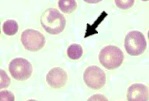
- Spherocytes are types of poikilocytes caused by a membrane abnormality. They are sphere shaped red blood cells due to damage to the membrane – commonly seen in AIHA/IMHA in hemolysis (also seen in hereditary spherocytosis). Spherocytes are RBCs that have not been completely removed from circulation by the spleen. The spleen takes off a portion of the RBC and it returns to circulation. These cells can indicate an autoimmune attack on RBCs and can be diagnostic for AIHA / IMHA. When a bit of a RBC is removed , it becomes more spherically shaped with a denser red color, thus they are called spherocytes.
- Schistocytes are types of poikilocytes caused by cell trauma & are also called schizocytes. They are in fact broken or fragmented pieces of red blood cell which indicates high fragility of red blood cells, hemolysis due to “mechanical” damage or severe burns. The presence of schistocytes on a blood smear can indicate DIC, micropathic hemolytic anemia, glomerulonephritis, and hemolytic anemia.The damage is caused to the red cells when they pass through or by fibrin strands, mesh or clot, shearing the cell membrane.
- Target cells are types of poikilocytes caused by membrane abnormality. There are many names for these including leptocytes, codocytes, Mexican hat cells, bulls eye cells. They indicate iron deficiency, liver disease, thalassaemia, inherited abnormal forms of haemoglobin (haemoglobinopathies).
- Stomatocytes are types of poikilocytes caused by a cell membrance abnormality. They are also called mouth cells & are seen in lead poisoning, thalassemia & hereditary stomacytosis.
- Sickle cells are types of poikilocytes caused by a cell membrance abnormality. They are also called drepanocytes & are sickle or crescent shaped cells due to hereditary sickle cell anemia.
- Semilunar bodies are types of poikilocytes caused by cell trauma. They are decolourised, crescent shaped cells, also called ghost corpuscles/cells or phantom cells. This erythrocyte cell is an “empty” red cell membrane (the external structure or “covering”) that is left complete or intact after hemolysis, but the cell is dead. In some cases of AIHA/IMHA, semilunar bodies/ghost erythrocytes may be seen with intravascular hemolysis.

















































































































































































































































































































